How can glucose (blood sugar) levels affect your general wellbeing?
Stable glucose levels are critical for maintaining overall health, even in people without diabetes. Learn how glucose monitoring can support your well-being.
Sarah Koenck, MS, RD,
Medical Affairs
Pamela Nisevich Bede, MS, RD, CSSD, LD,
Medical Affairs
Published:
December 27, 2024
Updated:
July 07, 2025
Read time:
7 minutes
Stable glucose levels are critical for maintaining overall health, influencing energy levels, mood, cognitive function, and sleep quality, even in individuals without diabetes.
Poorly managed glucose levels lead to significant short-term effects including increased hunger and cravings, diminished energy and focus, mood disturbances, and disrupted sleep patterns, which can impact daily well-being.
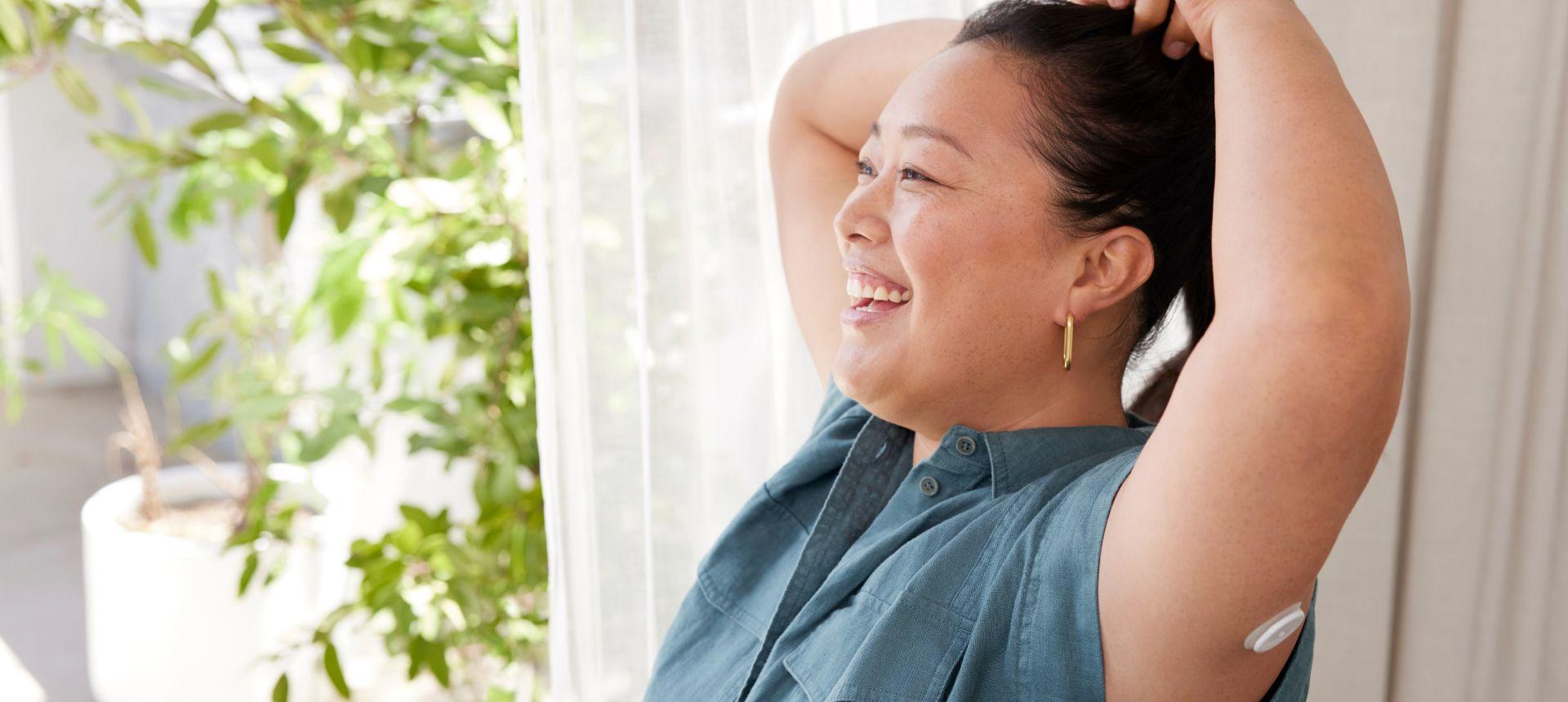
A continuous glucose monitor (CGM) can empower you to track your glucose directly on your smartphone, facilitating informed decisions about lifestyle habits that can optimize your overall health and well-being.
Start Lingo today for just $49
Learn how your body responds to food and exercise with a 2-week plan*, no commitment.
Buy now
In the journey towards optimal health and vitality, more and more research points towards the importance of stable glucose and the benefits of monitoring your glucose levels.1
While traditionally associated with diabetes management, monitoring glucose has proven health benefits, even for those who are not living with the condition. Understanding and regulating glucose levels can profoundly impact overall well-being, influencing hunger, energy levels, mood, sleep patterns, and more.1
In this article, we’ll dive into the connection between glucose and well-being and explore how maintaining steady glucose impacts your quality of life.
We’ll also shed light on how a continuous glucose monitor (CGM) can empower you to make informed decisions about your lifestyle habits and help you establish healthier behavior change to better your overall well-being.
Why your glucose levels matter, even without diabetes
Glucose serves as the primary source of energy for the body’s cells. Even if a diet contains zero carbohydrates, the body will produce its own glucose to maintain a steady stream in the blood.2 Maintaining stable glucose levels is crucial for sustained energy, mood regulation, cognitive function, and overall well-being.1
Of the three macronutrients — carbohydrates, protein, and fat — carbohydrates are what affect glucose levels the most. While different carbohydrates have different effects, a glucose spike will typically happen after eating a carb-heavy meal, especially if the carbohydrates are mostly simple carbs (e.g., white bread, pasta, sweets) or eaten alone (e.g., without a source of protein or fat).
While a modest increase in glucose after a meal is normal, it’s the large rises and crashes that cause problems.
Additionally, high-intensity exercise can cause a glucose spike because it increases hormones that release glucose into the system to fuel the activity.3 While this quick influx of fuel can spike your glucose, it is not something to be concerned about as the spike has a purpose — to fuel the activity — and tends to normalize after the activity is stopped.
In addition to diet and exercise, stress and sleep play a significant role in glucose regulation.4,5 Chronic stress can lead to increased glucose as the body releases stress hormones like cortisol and adrenaline, which stimulates glucose release into the bloodstream. Poor sleep quality or inadequate sleep duration can disrupt glucose metabolism, contributing to fluctuations in glucose levels.4
While many are aware that poorly managed glucose levels can lead to long-term complications such as heart disease and type 2 diabetes,1,6 the short-term effects are a little less known but still significant.
Large fluctuations in glucose as well as frequent glucose spikes can have a profound impact on day-to-day life impacting things like hunger and cravings, energy, mood, focus, sleep, and skin health.1,7
Benefits of stable glucose for your well-being
Many people are unaware that some of the symptoms they experience on a daily basis may be related to their glucose levels. Craving sweets in the afternoon, losing focus after lunch, feeling irritable during a meeting, or experiencing poor quality sleep can all be effects of poorly managed glucose.
Let’s explore five ways that stable glucose can have an impact on daily well-being:
1. Hunger and cravings
Research indicates that glucose spikes, followed by a crash, can intensify hunger and subsequent cravings for food.8 Conversely, when glucose remains steady, there tends to be less interest in food and fewer cravings.9 The cycle of increased hunger and cravings can disrupt daily activities, leading to erratic eating patterns and potential weight gain.10
2. Energy and focus
A study that looked at both mood and energy levels found that individuals following a high glycemic load (high GL) diet, characterized by its tendency to induce erratic blood glucose patterns, reported experiencing more fatigue compared with those adhering to a low glycemic load diet (low GL), known for promoting steadier glucose levels.11
Fluctuations in glucose levels can significantly impact energy levels and cognitive function. Following a spike in glucose, there is often a subsequent crash, leaving individuals feeling fatigued and moody.11
This rollercoaster effect not only impairs productivity and focus,12 but also hampers overall energy levels,13 making it challenging to sustain optimal performance throughout the day.
3. Mood
The same study found that individuals following the high GL diet saw a 38% higher score in depressive symptoms and 55% higher score in total mood disturbances than those following a low GL diet.11
Glucose levels play a crucial role in regulating mood, with fluctuations often leading to mood swings and irritability.
Recent research is pointing toward direct effects of both glucose levels and insulin and their effects on depression and mood.14,15 High and low blood glucose as well as higher than normal insulin levels can negatively impact your mood while steady glucose has been shown to have positive effects.1,11,14,15
4. Sleep
Poorly managed glucose levels can disrupt sleep quality, leading to difficulties falling asleep, frequent awakenings during the night, and overall restless sleep.16, 17 Poor sleep quality can disrupt essential restorative processes that can further impact mood, cognitive performance, and physical health.
Additionally, studies have found that not only do steady glucose levels help improve sleep quality but better sleep also helps improve glucose levels. Keeping your glucose steady may result in better sleep18 and a good night’s sleep may also help keep your glucose steady.4
5. Skin health
Glucose levels can also affect skin health, contributing to issues such as increased acne breakouts and skin inflammation. Fluctuations in blood glucose can stimulate the production of sebum, an oily substance that can clog pores and lead to acne.7
Additionally, elevated glucose can promote inflammation, exacerbating skin conditions such as eczema and psoriasis.19 This added burden of skin issues can further affect self-esteem and overall well-being.
Monitoring your glucose levels with a CGM
Persistent fluctuations in glucose levels not only disrupt your body’s natural rhythm, but also contribute to a range of symptoms that can significantly diminish your quality of life. Recognizing and addressing these interconnected factors is essential for taking control of your health and finding balance in your daily life.
To cultivate a deeper awareness of your body’s glucose levels and optimize your well-being, there are several strategies you can implement.
Firstly, maintaining a balanced diet rich in whole foods, protein, and fiber while minimizing refined sugars and processed carbohydrates can help stabilize glucose.
Regular physical activity is also crucial, as exercise can enhance insulin sensitivity and promote glucose regulation.
Furthermore, paying attention to how different foods and lifestyle factors impact your energy levels, mood, hunger cues, and sleep can provide valuable insights into your body’s responses to glucose fluctuations. Keeping a food diary and tracking symptoms can help identify patterns and find the foods and lifestyle habits that help stabilize your glucose.
Lingo is a CGM that’s designed to give you an even greater understanding of your own glucose patterns and support proactive changes to your daily habits that can help promote steady glucose.
Gaining access to insights on how your food choices and daily habits affect your glucose can allow you to make informed decisions about your diet, physical activity, mood, and sleep to help you better optimize your overall well-being.
A final note from Lingo
Paying attention to how your food choices and other lifestyle factors impact your energy, mood, cravings, and sleep can help you gain clarity into what might be impacting your glucose patterns the most.
Lingo is designed to offer personal insights into these glucose responses, empowering you to make lifestyle changes to improve your quality of life and overall well-being.
With increasingly more research pointing towards the importance of steady glucose for short-term and long-term health, integrating healthier strategies into your lifestyle can help cultivate a deeper connection with your body and foster greater balance and overall health.
The Lingo Glucose System is intended for users 18 years and older not on insulin. It is NOT intended for diagnosis of diseases, including diabetes.
The Lingo program does not guarantee that everyone will achieve the same results as individual responses may vary. Consult your healthcare professional before making changes to your diet or exercise regimen or if you have an eating disorder or a history of eating disorders.
© 2026 Abbott. All rights reserved. The biosensor shape and appearance, Lingo, and related brand marks are marks and/or designs of the Abbott group of companies in various territories. Other marks are the property of their respective owners.
ALB-02189
Published:
December 27, 2024
Updated:
July 07, 2025
Read time:
7 minutes


Sarah Koenck, MS, RD, is a Medical Affairs Specialist at Lingo. She’s been a registered dietitian since 2011 and has a master's degree in kinesiology from A.T. Still University. She spent the first part of her career as a clinical dietitian in the ICU before moving onto specializing in diabetes and weight management in the digital health space. Her personal health journey, including living with type 1 diabetes for almost 30 years and wearing a continuous glucose monitor for almost 20, has driven her commitment to help others at Lingo.


Pamela Nisevich Bede, MS, RD, CSSD, LD, is a certified specialist in sports dietetics and an expert in nutrition communications. Pam earned her Bachelor of Science degree in Dietetics from Miami University and a Master of Science in Medical Dietetics from The Ohio State University. While at Abbott Nutrition, Pam was the Global Nutrition Lead at Zone Perfect Nutrition and Ensure and was previously the Manager of Nutrition Marketing at EAS Sports Nutrition.
More to explore on the blog

What is a CGM? How it works and how to apply one
Continuous glucose monitors (CGMs) are wearable devices that measure your glucose levels around the clock. Learn why people with and without diabetes are using CGMs.
April 04, 2025|7 minutes

What is a glucose spike?
The causes, symptoms, effects, and how to manage them for better metabolic health.
December 09, 2024|10 minutes
A healthy choice for your inbox
Sign up for Lingo emails to get science-backed tips, special offers, and The Journey Newsletter.
Start Lingo today
for just $49
Learn how your body responds to food and exercise with a 2-week plan*, no commitment.
- 1 Lingo biosensor with minute-by-minute glucose monitoring.
- Full access to the Lingo app.
- Available over the counter. No prescription needed.
- Works with iOS and AndroidTM
Shop now
Free shipping | 30-day money-back guarantee†
*No commitment. This plan does not auto-renew.
†30-day money-back guarantee is for first time purchases only

