How high blood glucose levels can impact heart health
Consistently high glucose (blood sugar) levels can raise heart disease risk. We share 10 science-backed tips for glucose and heart health.
Andrea Givens, MS, RD, CSSD,
Medical Affairs
Sarah Koenck, MS, RD,
Medical Affairs
Published:
August 20, 2025
Read time:
9 minutes
Heart and circulatory diseases are a leading cause of death for men and women in the UK, causing a quarter of all deaths each year and killing one person every 3 minutes.1
Studies consistently show a strong link between glucose health and heart health, even in individuals without diabetes.2,3,4,5
This article explains this connection, plus what you can do to improve your cardiometabolic health: the combined health of your heart and metabolism.
Let’s break it down:
Heart health and metabolic health are closely linked, and both are important for overall health.
Keeping glucose in a healthy range helps prevent chronic conditions such as type 2 diabetes, which is better for heart health.
We’ve outlined 10 expert tips to help manage glucose levels and improve your heart health.
Start Lingo today for just £59
Learn how your body responds to food and exercise with a 2-week plan*, no commitment.
Buy now
What does glucose (blood sugar) have to do with heart health?
Glucose levels rise in response to the breakdown of the carbohydrates you eat, or from the release of stored glucose (glycogen) in the body. As glucose rises, insulin, a hormone made by the pancreas, is secreted.
Insulin acts like a key that unlocks cells, which allows glucose to move from the blood into cells where it’s used for energy or stored for later use. Insulin also signals to the liver to stop releasing glucose into the bloodstream.
This negative feedback loop works repeatedly to keep glucose levels steady, maintaining them in a narrow range that keeps the body functioning well. In someone with good metabolic health, this system functions efficiently, allowing glucose to fluctuate but keeping it in a healthy range.
However, some people experience resistance to the effects of insulin. As a result, the pancreas must produce more insulin to maintain glucose levels within this range.
Over time, when the amount of insulin produced can no longer compensate, more time is spent above the healthy range and overall glucose levels rise.
Consistently elevated glucose levels, even those not high enough yet to be diagnosed as diabetes, are linked to greater risk of heart disease.2,3,6,7
High fasting blood glucose is often clustered with other markers of poor metabolic health, including:
High triglycerides.
Low HDL (“good”) cholesterol.
High blood pressure.
Larger waist circumference.
When a person has at least 3 out of 5 of these markers, they’re diagnosed with metabolic syndrome,8 which is linked to a higher risk of diabetes and heart disease.9
Lifestyle habits like eating less ultra-processed food, filling up on non-starchy vegetables, and strength training can all benefit your glucose and heart health.
Insulin resistance: a silent strain on the heart
What to know:
- Insulin resistance affects how your body takes up glucose in the blood.
- Insulin resistance can be one component of metabolic syndrome, which is linked to a higher risk of diabetes and heart disease.
- Insulin resistance damages heart health by changing the way the body metabolizes fats in the blood.
- Insulin resistance is thought to have many contributing factors, including excess carbs in the diet,10 physical inactivity,10 and genetics.14
One component of metabolic syndrome is insulin resistance10 — when cells in your muscles, fat, and liver don't respond well to insulin and can't efficiently take up glucose from your blood.11
Insulin resistance likely stems from multiple factors, including:
Too much sugar or carbohydrate in the diet over time.10
Physical inactivity.10
Excess body fat (especially accumulation around the organs).12
Inflammation.13
Genetics.14
One way insulin resistance damages heart health is by changing the way the body metabolises fats in the blood.15
This disruption can lead to increased triglycerides and VLDL (“bad”) cholesterol, and low HDL (“good”) cholesterol. It can also set the stage for creating a lipid pattern that’s considered harmful for the heart.15,16
These changes contribute to plaque formation in the arteries — a characteristic of atherosclerosis (a type of heart disease).16
Persistently elevated insulin levels can promote blood clot formation and raise the risk of heart attacks.17
Insulin resistance can also impact how well your blood vessels work. Normally, healthy blood vessels relax and constrict, moving oxygen and nutrients through the body.
Insulin resistance can reduce blood vessels’ ability to relax and cause stiffness to smooth cardiac muscle. This increases blood pressure and promotes blood vessel damage.18
Research shows a direct link between insulin resistance and the risk of developing both prediabetes and type 2 diabetes, (16,19) both of which are strongly associated with an increased risk of heart disease.4
Currently, measuring insulin is only available in a clinical setting — not with any at-home tests.
Elevated glucose raises heart disease risk
Research also shows a connection between glucose levels and risk of heart disease. A study involving nearly 20,000 adults found that as HbA1c levels (a measure of average glucose control over the past ~3 months) exceeded 5.5% — just below the prediabetes diagnosis of 5.7% — the risk of dying from heart disease increased.5
Fortunately, maintaining good glucose health and keeping glucose mostly within the healthy range is linked to less risk of developing type 2 diabetes or heart disease.20,4
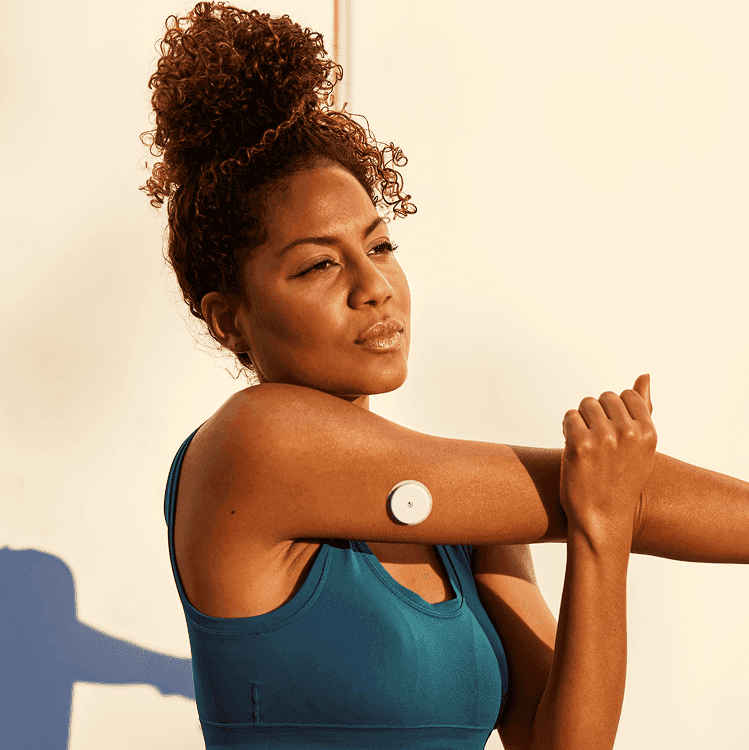
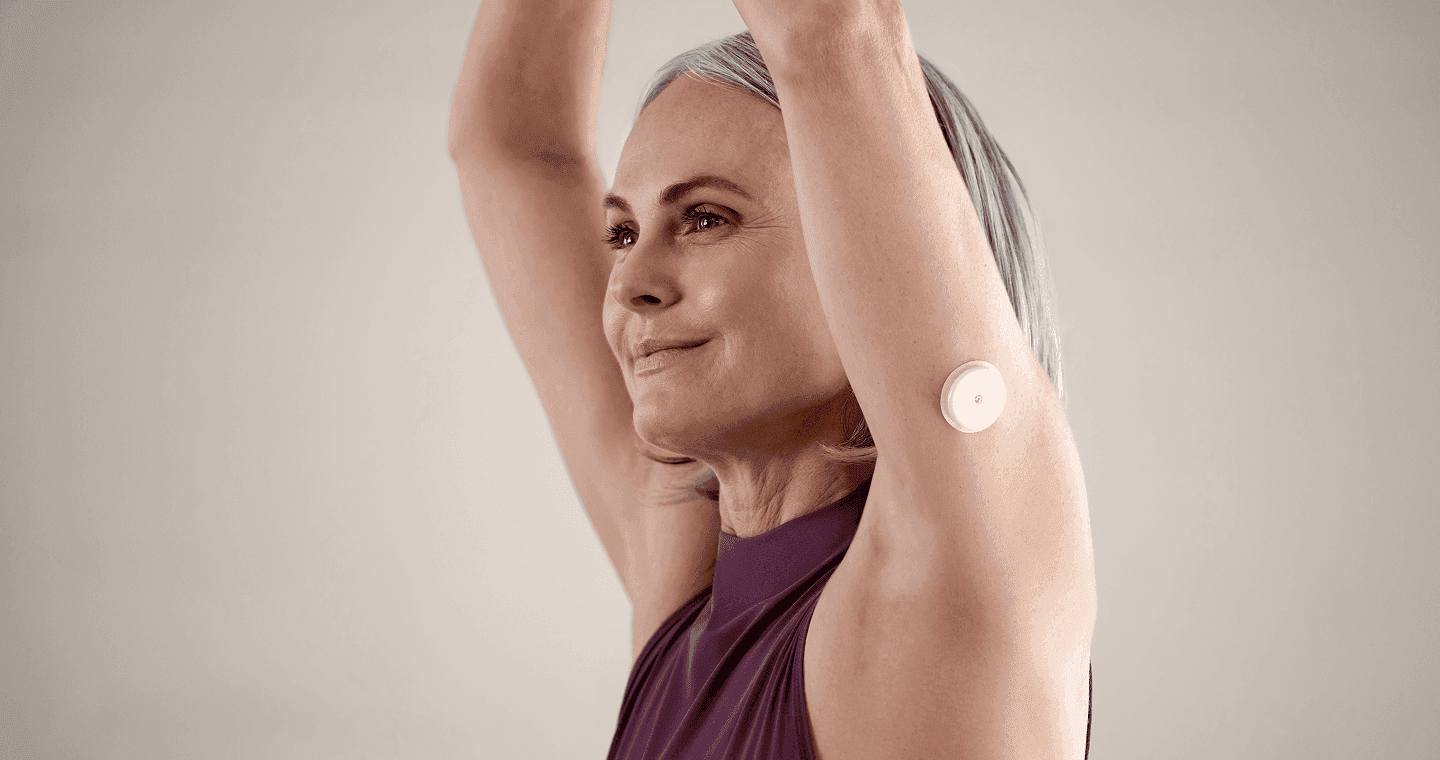
You can help maintain or improve glucose health with certain lifestyle strategies, including using a continuous glucose monitor (CGM). Consumer CGMs, such as Lingo, are gaining mainstream popularity and are now available without a prescription.


Staying in a healthy glucose range can help keep your heart healthy,[3,4,5] and using a CGM has been shown to help people stay in a healthy glucose range more often.[22]
Health benefits of wearing a CGM
Studies have shown that even if you don’t have diabetes, wearing a CGM to help adopt healthier habits can improve overall glucose patterns.22,23 Maintaining healthy glucose levels is linked to a lower risk of developing type 2 diabetes20 and heart disease.4,21
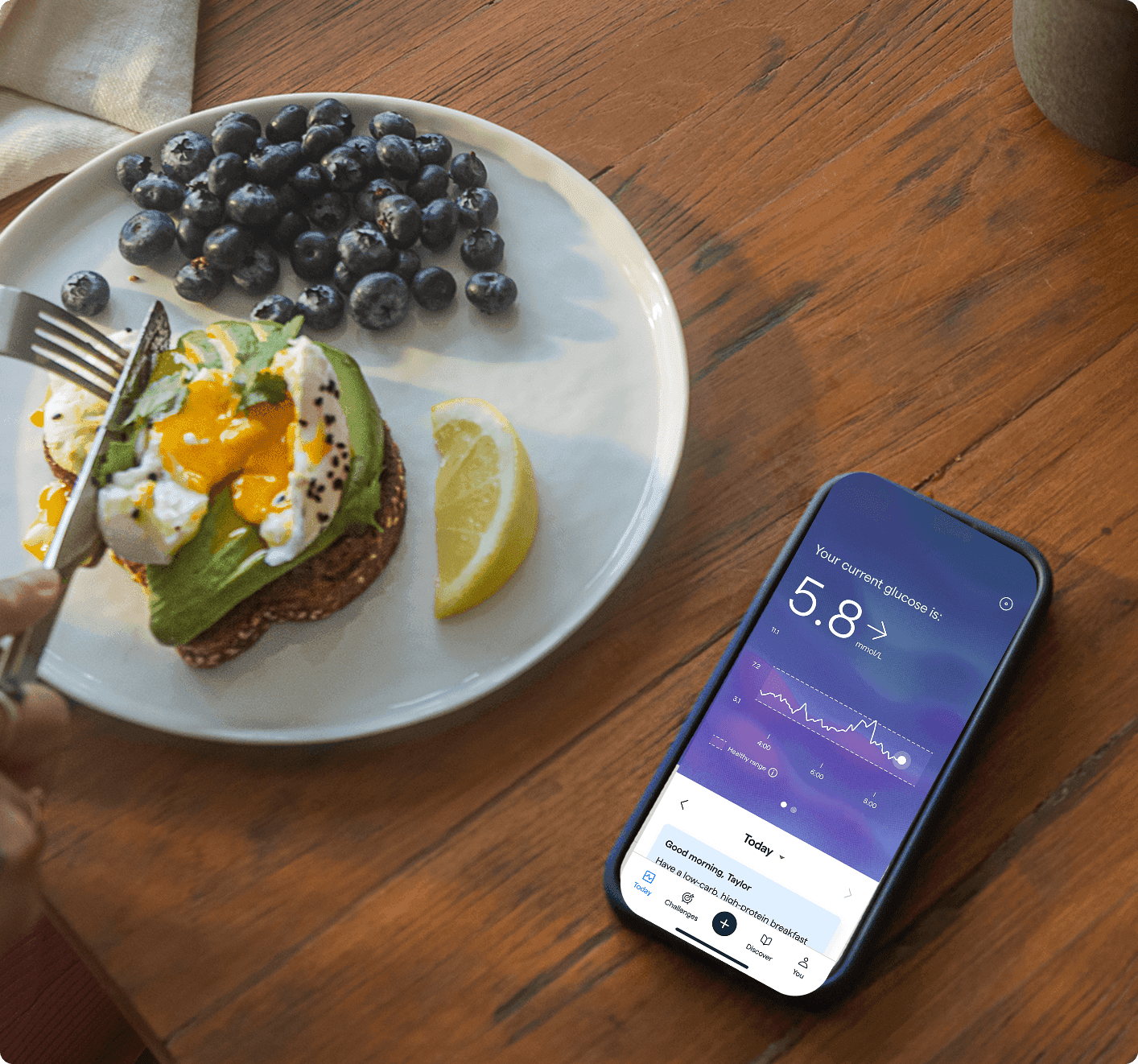
Lingo tracks your glucose in real time, which can help connect how diet, exercise, and stress impact your glucose. Along with helpful prompts, the Lingo app includes a more simplified look at your glucose data to help you better understand your unique responses and how lifestyle factors play a role.
With these insights, you can learn the strategies that work best for your body to keep glucose levels in a healthy range and help improve overall health and wellbeing.
It’s important to note that Lingo is not to be used for the diagnosis or treatment of any disease, including diabetes.


10 tips for cardiometabolic health from Lingo experts
Don’t smoke. Smoking cigarettes negatively impacts cardiometabolic health in several ways, primarily by causing poor blood vessel health, inflammation, insulin resistance, and disruption of lipid profiles.24,25
Cannabis use has also been linked to increased risk of heart attack, stroke, and heart failure, with some studies showing a stronger association in younger individuals and heavier use (more days per month).26
Seek a smoking cessation program and, if quitting cigarettes or tobacco products, consider if nicotine replacement therapy is right for you.
Limit alcohol. Alcohol consumption at all levels has been associated with increased risk of cardiovascular disease27 and can contribute to unsteady glucose.28 The NHS recommends drinking no more than 14 units of alcohol a week, spread across three or more days.29
Follow a low-glycaemic diet. High carbohydrate intake, and specifically high GI foods known to spike glucose more, have been linked to an increased risk of heart disease through changes in lipid metabolism and high triglycerides.30,31
Build your meals around protein, healthy fats, and non-starchy vegetables or foods with low-GI carbs to help keep glucose levels in the healthy range.
Strength train. Studies suggest strength training reduces risk of heart disease by increasing muscle mass and decreasing body fat (specifically visceral fat), improving glucose control, metabolic dysfunction, and inflammation.32
Incorporate compound movements that work major muscle groups to your routine at least twice a week, such as squats, lunges, bench press, or push-ups.
Fill half your plate with non-starchy vegetables like leafy greens, which are packed with fibre. Fibre helps slow digestion, manage glucose, and helps you feel more satiated.33,34

Fill half your plate with non-starchy vegetables like leafy greens, which are packed with fibre. Fibre helps slow digestion, manage glucose, and helps you feel more satiated.[33,34]
Fill up on fibre-rich foods. Leafy greens and non-starchy vegetables (like broccoli, kale, carrots, and asparagus) are packed with healthy fibre, which helps slow digestion, manage glucose levels, and helps you feel more satiated.33,34 Add colour to every meal with a variety of vegetables.
Incorporate cardio exercise. Studies show that active people who engage in cardiovascular exercise (like jogging, swimming, biking — activity that gets your heart rate up) have lower blood pressure, higher insulin sensitivity, and healthier levels of fats and cholesterol in their blood.33 Aim for 30 minutes of moderate-intensity exercise at least 5 days per week.
Limit ultra-processed food. Ultra-processed foods are often full of added sugars and unhealthy fats that can negatively impact cardiometabolic health when eaten in excess.36,37 These foods are designed to be highly palatable (extremely tasty and hard to resist).38 Stock up on minimally processed snacks like nuts and crudités.
Manage stress. Stress contributes to the long-term development of heart disease as well as acute triggering of cardiac events.39 Find moments to de-stress, like breathing exercises, guided meditations, or gathering with family and friends.
Don’t fear fat. Swapping saturated fat in the diet for refined carbohydrates doesn’t prevent heart disease. In fact, studies show adverse effects like decreased insulin sensitivity and unfavorable cholesterol levels.40,41 Fat is an important part of your diet, so include heart-healthy fats like avocado, full-fat dairy, nuts, seeds, and fatty fish.
Get enough Zzs. Lack of sleep increases sympathetic nervous system activity and blood pressure, which contribute to heart disease.42 Aim for 7-9 hours per night.

A final note from Lingo
Staying in a healthy glucose range can help keep your heart healthy,3,4,5 and using a CGM has been shown to help people stay in a healthy glucose range more often.22 Lingo is a biowearable CGM system designed to help you understand your body’s glucose response to food, activity, sleep, and more.
Lingo members who reduced their Lingo Count — the proprietary algorithm and value used to measure glucose spikes — over the course of six sensors (about three months) also spent less time above the healthy glucose range.43
Using your unique glucose data, Lingo empowers you to make healthier choices to help benefit your overall health and wellbeing.23,44
The Lingo Glucose System is intended for users 18 years and older not on insulin. It is NOT intended for diagnosis of diseases, including diabetes.
The Lingo program does not guarantee that everyone will achieve the same results as individual responses may vary. Consult your healthcare professional before making changes to your diet or exercise regimen or if you have an eating disorder or a history of eating disorders.
© 2026 Abbott. All rights reserved. The biosensor shape and appearance, Lingo, and related brand marks are marks and/or designs of the Abbott group of companies in various territories. Other marks are the property of their respective owners.
ALB-02852 v2.0
Published:
August 20, 2025
Read time:
9 minutes


Andrea Givens, MS, RD, CSSD, is a Senior Medical Affairs Specialist and Health Coach at Lingo. Andrea has a passion for empowering individuals to leverage their unique physiology to optimize performance and health. She’s been a registered dietitian since 2010 and has been a board-certified specialist in sports dietetics since 2017. She holds master's degrees in both nutrition science and exercise physiology from San Diego State University.


Sarah Koenck, MS, RD, is a Medical Affairs Specialist at Lingo. She’s been a registered dietitian since 2011 and has a master's degree in kinesiology from A.T. Still University. She spent the first part of her career as a clinical dietitian in the ICU before moving onto specializing in diabetes and weight management in the digital health space. Her personal health journey, including living with type 1 diabetes for almost 30 years and wearing a continuous glucose monitor for almost 20, has driven her commitment to help others at Lingo.
More to explore on the blog

What is a glucose spike?
The causes, symptoms, effects, and how to manage them for better metabolic health.
December 09, 2024|10 minutes
Does metabolism actually slow down with age?
What you need to know about how aging impacts your metabolism, according to research.
December 09, 2024|10 minutes